Isolation and Antibiotic Susceptibility of Escherichia coli from Urinary Tract Infections
| Received 30 Nov, 2023 |
Accepted 11 Feb, 2024 |
Published 30 Jun, 2024 |
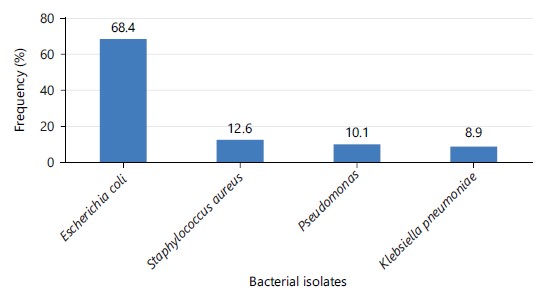
Background and Objective: Escherichia coli is the most prevalent bacteriological agent responsible for Urinary Tract Infections (UTIs) in humans, as well as the most common nosocomial infection in developed countries. The broad availability of antimicrobial drugs has made them difficult to treat due to the emergence of infections with rising antibiotic resistance. The study was carried out in a tertiary care hospital in Sirajganj on a urinary tract infection with Escherichia coli for isolation and diagnosis of antibiotic resistance. Materials and Methods: Urine samples (n = 296) were obtained from patients exhibiting signs and symptoms of urinary tract infections. Bacteria were extracted and identified using conventional biochemical techniques. The Kirby-Bauer method was used to determine E. coli resistance to various antibiotics. Results: A bacterial etiological agent was recovered from 79 samples, with E. coli having he ighest revalence 54, 8.4%), ollowed y taphylococcus ureus 12.6%), Pseudomonas species (10.1%) and Klebsiella species (8.9%). The Escherichia coli was highly resistant to Ceftazidime (85.2%), Ceftriaxone (72.2%), Amoxycillin (68.5%) and Nalidixic acid (64.8%), followed by intermediate resistance to Cefuroxime (59.3%), Netilmicin (51.9%), Azithromycin (50.0%) and Ciprofloxacin (40.7%) and low resistance to Gentamycin (31.5%), Nitrofurantoin (27.8%) and Imipenem (13.0%). Out of 79 Escherichia coli isolates, 60 (75.9%) were declared as multiple drug-resistant and 2 (2.5%) were extensive drug-resistant. Conclusion: It has been determined that multiple medication-resistant Escherichia coli is to blame for the majority of human urinary tract infections.
INTRODUCTION
Urinary tract infections are one of the leading causes of morbidity and mortality. Escherichia coli is the most common urinary pathogen, accounting for 50-90% of all uncomplicated urinary tract infections.
Escherichia coli in the gastrointestinal tract as commensals supply the pool for the beginning of UTI. The UTIs are serious health problems that affect people all over the world. In Bangladesh, Urinary Tract Infections (UTIs) are extremely common1.
Escherichia coli was the most common uropathogen, followed by Klebsiella pneumoniae and Pseudomonas aeruginosa. Females were more likely than males to have UTIs and both were more common in the middle age groups. Gentamicin, Imipenemand Meropenem were discovered to be effective treatments for the examined uropathogens due to their broad spectrum of activity in the current investigation. Antibiotic selection for UTI must be guided by culture and sensitivity testing and empirical medicines must be chosen based on recent antibiograms from a specific geographical area2.
The most frequent bacteria that cause UTIs in humans are Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, Staphylococcus saprophyticus, Staphylococcus aureus and Proteus mirabilis. The most predominant Gram-negative isolate was E. coli (96.2%) and the rest of the isolates were Klebsiella pneumoniae 1 (1.9%) and Pseudomonas aeruginosa 1 (1.9%)2,3.
Urinary Tract Infection (UTI) is one of the most common infections afflicting people of all ages and genders. About 85% of UTIs obtained in the community and 50% of UTIs acquired in hospitals are caused by E. coli4. Several variables, including urological equipment, immunosuppression, age and gender, may influence the frequency of UTIs5. One of the most serious health hazards, catheter-associated UTIs account for 34% of all infections related to healthcare6.
The empirical use of cephalosporins and Ciprofloxacin has been put in jeopardy by the advent of extended-spectrum beta-lactamases7. Different processes, including horizontal gene transfer, recombination of foreign DNA in bacterial chromosomes and genetic material modification, are used by microorganisms to build drug resistance8. Microorganisms’ resistance patterns differ from nation to nation, state to state, large hospital to small hospital and hospital to community.
The overuse and abuse of antibiotics in Bangladesh are contributing to the problem of antibiotic resistance5,9. Inadequate data are available to quantify the issue and there is no regular national surveillance of antibiotic resistance10. To improve the efficacy of empirical treatment, it is critical to identify the bacteria that cause UTIs and evaluate whether they are resistant to commonly used antibiotics11-13. The goal of the current investigation was to shed light on the bacterial causes of urinary tract infections and identify the E. coli isolates’ patterns of resistance.
MATERIALS AND METHODS
Study area: The study was conducted at the Health Aid Diagnostic and Consultation Center, Sirajganj, which is one of the oldest and biggest diagnostics centers in Sirajganj between January, 2023 to June, 2023.
Sample collection and isolation of bacteria: The urine samples (n = 296) were obtained from patients of various ages. The samples were centrifuged and the sediments were grown principally on blood agar and MacConkey’s agar using the stick plate technique. Bacterial colonies of various morphologies were chosen, purified and identified based on their biochemical profiles.
Multiple drug resistance: Antibiotic sensitivity of E. coli isolates was evaluated on Muller-Hinton agar plates using Kirby-Bauer disc diffusion14. Isolates were declared sensitive or resistant based on the zone of inhibition following the criteria of the Clinical Laboratory Standards Institute14.
Ethical consideration: The ethical approval was taken from the ethical grant committee at Khwaja Yunus Ali University. Refrence No: KYAU/DEAN/EGC/2023/007.
RESULTS AND DISCUSSION
A total of 296 cases of different ages and sex those who fulfilled the inclusion criteria of suspected UTI were included in this study. Out of 296 cases, 79 cases were positive and 217 cases were negative. The rates of positive and negative cases in isolated urinary tract pathogens were 26.7 and 73.3%, respectively. Among the culture of 296 urine samples, E. coli was the predominant isolate at 54 (68.4 %), as presented in Fig. 1.
The bacterial etiology of Urinary Tract Infections (UTIs) in outpatient at the Health Aid Diagnostic and Consultation Center, Sirajganj, was determined. The resistance pattern of E. coli against several antibiotics was also checked. Bacteria were successfully isolated from 79/296 samples. The rate of isolation of bacterial etiological agents from female samples (78.2%) was not significantly higher as compared to male (41.8%) patients. Out of 79 bacterial isolates from patients, the rate of E. coli (54, 68.4%) isolation was the highest, followed by Staphylococcus aureus (12, 12.6%), Pseudomonas species (8, 10.1%) and Klebsiella species (7, 8.9%) (Fig. 1).
Escherichia coli exhibited the highest resistance to Ceftriaxone (85.2%), followed by Ceftriaxonee (72.2%), Amoxycillin (68.5%), Nalidixic acid (64.8%), Cefuroxime (59.3%), Netilmicin (51.9%), Azithromycin (50.0%), Ciprofloxacin (40.7%), Gentamycin (31.5%), Nitrofurantoin (27.8%) and the lowest resistance to Amikacin, Imipenem(13.0%). Table 1 out of 79 E. coli isolates, 60 (75.9%) were multiple drug resistant and 2 isolates were extensively drug resistant. Multiple drug resistance was defined as resistance to three or more of the three different antibiotic classes tested.
The UTIs are brought on by bacterial invasion and subsequent proliferation in the urinary tract. Other findings were supported by the fact that although female patients (78.2%) had a higher infection rate than male patients (41.8%), this difference was correlated with Shah et al.15.
Iqbal et al.5 reported that older patients (>50 years) had a greater rate of bacterial isolation. Escherichia coli was discovered to be the most common etiologic agent of UTI, which was also consistent with other findings16-18. Among the most important scientific discoveries of the twentieth century were antibiotics, which are used to either kill or stop the development of germs. There is a severe public health concern due to the increased incidence of antibiotic resistance in E. coli isolated from UTIs. It is essential to recognize the patterns of antibiotic resistance in E. coli isolates to make sure those prescriptions are suitable and precise.
|
| Table 1: | Antibiotic sensitivity pattern of Escherichia coli isolates | |||
Patterns |
|||||||
Sensitive |
Intermediate |
Resistant |
|||||
| Antibiotics | Disks concentration |
n |
(%) |
n |
(%) |
n |
(%) |
| Amikacin | 30 μg |
39 |
72.2 |
8 |
14.8 |
7 |
13.0 |
| Amoxycillin | 20 μg |
11 |
20.4 |
6 |
11.1 |
37 |
68.5 |
| Azithromycin | 10 μg |
19 |
35.2 |
8 |
14.8 |
27 |
50.0 |
| Ceftazidime | 30 μg |
3 |
5.6 |
5 |
9.3 |
46 |
85.2 |
| Ceftriaxonee | 30 μg |
10 |
18.5 |
5 |
9.3 |
39 |
72.2 |
| Cefuroxime | 30 μg |
13 |
24.1 |
9 |
16.7 |
32 |
59.3 |
| Ciprofloxacin | 5 μg |
28 |
51.9 |
4 |
7.4 |
22 |
40.7 |
| Imipenem | 10 μg |
45 |
83.3 |
2 |
3.7 |
7 |
13.0 |
| Netilmicin | 15 μg |
19 |
35.2 |
7 |
13.0 |
28 |
51.9 |
| Nitrofurantoin | 20 μg |
35 |
64.8 |
4 |
7.4 |
15 |
27.8 |
| Gentamycin | 10 μg |
29 |
53.7 |
8 |
14.8 |
17 |
31.5 |
| Nalidixic acid | 30 μg |
9 |
16.7 |
10 |
18.5 |
35 |
64.8 |
| N: Number and %: Percentage | |||||||
The UTIs caused by bacteria that are both antibiotic and multi-drug-resistant have increased in recent years. The UTI difficulties have increased as a result of the spread of bacterial infections that generate Extended-Spectrum Beta-Lactamases (ESBL), which are also to blame for a variety of therapeutic and epidemiological issues. Nearly ten years ago, Klebsiella spp. dominated the nosocomial ESBL-producing microbial population, but the problem has recently worsened due to the presence of ESBL and MDR Escherichia coli. The majority of ESBL E. coli are resistant to a variety of beta-lactamase drugs, including Cephalosporins, Penicillin and Piperacillin/Tazobactam, as well as several non-beta-lactamase treatments such as Fluoroquinolones, Trimethoprim and Gentamycin19.
All 54 isolates of E. coli species tested in the current study were resistant to Ceftazidime and Ceftriaxone, indicating that these medicines should only be used with caution to treat urinary tract infections. Escherichia coli resistance to the Ceftazidime group of antibiotics has been on the rise and is rising daily in many regions of the world; however, there are only a small number of cases that suggest 90% resistance to Ceftazidime20. Resistance to amoxicillin and a beta-lactamase inhibitor in combination was also quite high. Beta-lactam inhibitors have been shown in prior research to boost the effectiveness of the Ceftazidime category of antibiotics against E. coli. Other beta-lactam antibiotics such as Cefotaxime (89.7%), Ceftazidime (73.8%), Cefuroxime (58.26%) and Ceftriaxone (43.3%) were resistant to some extent21. Other beta-lactamase antibiotics, such as Cefotaxime (89.7%), Ceftazidime (73.8%), Cefuroxime (58.26%) and Ceftriaxone (43.3%), also have very high rates of resistance, making many of them ineffective for use as empirically prescribed UTI treatments. Escherichia coli has a very high level of antibiotic resistance to cephalosporins and Ceftazidime, according to earlier investigations conducted in Bangladesh22.
Present study findings indicate that Ceftazidime and Ceftriaxone shouldn’t be used to treat UTIs since they are often ineffective against UTI infections in impoverished nations like Bangladesh. Ceftazidime and Ceftriaxone’s ineffectiveness in this study does not mean that these antibiotics are not used elsewhere in the globe to treat UTIs brought on by E. coli. More E. coli was identified in some recent reports to be susceptible to Ceftazidime and Ceftriaxone from European nations23. These medicines were effective against E. coli even in Bangladesh a decade earlier20.
In comparison to past studies, this study discovered that E. coli exhibited higher resistance to Azithromycin and Ciprofloxacin at 50.0 and 40.7%, respectively23,24. Increased carbapenem resistance in E. coli raises the possibility that these medications were abused and/or misused in healthcare settings. The most effective treatment for UTIs was Netilmicin, a mixture of Piperacillin and the beta-lactamase inhibitor Gentamycin, for which E. coli resistance was only 26.7%, proving that this antibiotic is still useful in treating UTIs19-22. Escherichia coli was extremely resistant to Ceftazidime (85.2%) and Ceftriaxone (72.2%), even though the Ceftazidime group of antibiotics is no longer used to treat human pathogenic pathogens. For the aminoglycosides, varied resistance patterns were discovered in the current investigation. Gentamycin was extremely resistant to E. coli, whereas Nitrofurantoin (27.8%), Imipenem and Amikacin (13.0%) had modest levels of resistance.
Recently, E. coli infections have been treated with quinolones, notably Ciprofloxacin. Contrary to past findings, the current analysis discovered that E. coli exhibited a significant level of Ciprofloxacin resistance (54.2%)24. Additional studies from different regions of the world show that quinolones are still beneficial against UTI infections. The words extended drug resistance (XDR) and multiple drug resistance (MDR) were also mentioned in this study.
The MDR is defined as resistance to at least one member of three separate antibiotic classes that are used to treat E. coli, whereas extensive drug resistance (XDR) is defined as resistance to at least one member of all but two antibiotic classes. The MDR and XDR E. coli made up 85.2 and 13.0%, respectively, of the samples used in this analysis. The antibiotics that were commonly successful against the XDR were Amikacin and Imipenem.
CONCLUSION
Escherichia coli exhibits greater levels of MDR and XDR antibiotic resistance. Combination therapy, notably with Amikacin and Ciprofloxacin, may be more effective in treating UTIs brought on by Escherichia coli. Escherichia coli with antibiotic resistance seen in UTIs suggests strict monitoring and antibiotic prescriptions following culture sensitivity tests.
SIGNIFICANCE STATEMENT
Understanding the isolation and antibiotic susceptibility of Escherichia coli (E. coli) in Urinary Tract Infections (UTIs) is of paramount significance. Escherichia coli is a predominant pathogen causing UTIs and its behavior in response to antibiotics greatly influences treatment efficacy. This research provides essential insights into the prevalence, characteristics and antibiotic resistance patterns of E. coli in UTIs, contributing to evidence-based clinical practices. The findings will guide healthcare professionals in selecting optimal treatment strategies, combating antibiotic resistance and enhancing patient outcomes in the management of UTIs.
REFERENCES
- Lee, D.S., S.J. Lee and H.S. Choe, 2018. Community-acquired urinary tract infection by Escherichia coli in the era of antibiotic resistance. BioMed Res. Int., 2018.
- Abedin, M.Z., M.O. Faruque, M.S. Uz Zaman, R. Nasim and R. Hasan et al., 2020. Prevalence and in vitro antibiogram patterns of urinary tract pathogens in rural hospitals in Bangladesh. J. Chem. Biol. Phys. Sci., 10: 401-409.
- Boye, A., P.M. Siakwa, J.N. Boampong, G.A. Koffuor and R.K.D. Ephraim et al., 2012. Asymptomatic urinary tract infections in pregnant women attending antenatal clinic in Cape Coast, Ghana. E3 J. Med. Res., 1: 74-83.
- Ramanath, K.V. and S.B. Shafiya, 2011. Prescription pattern of antibiotic usage for urinary tract infection treated in a rural tertiary care hospital. Indian J. Pharm. Pract., 4: 57-63.
- Iqbal, T., R. Naqvi and S.F. Akhter, 2010. Frequency of urinary tract infection in renal transplant recipients and effect on graft function. J. Pak. Med. Assoc., 60: 826-829.
- Fink, R., H. Gilmartin, A. Richard, E. Capezuti, M. Boltz and H. Wald, 2012. Indwelling urinary catheter management and catheter-associated urinary tract infection prevention practices in Nurses Improving Care for Healthsystem Elders hospitals. Am. J. Infect. Control, 40: 715-720.
- Pondei, K., O. Oladapo and O.E. Kunle-Olowu, 2012. Anti-microbial susceptibility pattern of micro-organisms associated with urinary tract infections in a tertiary health institution in the Niger Delta Region of Nigeria. Afr. J. Microbiol. Res., 6: 4976-4982.
- Klemm, P., V. Roos, G.C. Ulett, C. Svanborg and M.A. Schembri, 2006. Molecular characterization of the Escherichia coli asymptomatic bacteriuria strain 83972: The taming of a pathogen. Infect. Immun., 74: 781-785.
- Tanvir, R., R. Hafeez and S. Hasnain, 2012. Prevalence of multiple drug resistant Escherichia coli in patients of urinary tract infection registering at a diagnostic laboratory in Lahore, Pakistan. Pak. J. Zool., 44: 707-712.
- Sabir, S., A.A. Anjum, T. Ijaz, M.A. Ali, Muti Ur Rehman and M. Nawaz, 2014. Isolation and antibiotic susceptibility of E. coli from urinary tract infections in a tertiary care hospital. Pak. J. Med. Sci., 30: 389-392.
- Ko, M.C., C.K. Liu, L.C. Woung, W.K. Lee and H.S. Jeng et al., 2008. Species and antimicrobial resistance of uropathogens isolated from patients with urinary catheter. Tohoku J. Exp. Med., 214: 311-319.
- Abedin, M.Z., F.A. Koly, M. Babul Aktar, M. Irfanul Islam and M. Anisur Rahaman et al., 2022. Prevalence and antimicrobial susceptibility pattern of pathogens isolated from different age groups with urinary tract infection at Tangail, Bangladesh. SSR Inst. Int. J. Life Sci., 8: 3044-3052.
- Mia, S., M. Babul Aktar, A.A. Laboni, S.A.R. Rahman and S. Akter et al., 2022. Bacteriological frequency and antibiotic susceptibility patterns of urinary tract infection in children, Sirajganj Sadar. Khwaja Yunus Ali Univ. J., 6: 18-23.
- Bauer, A.W., W.M.M. Kirby, J.C. Sherris and M. Turck, 1966. Antibiotic susceptibility testing by a standardized single disk method. Am. J. Clin. Pathol., 45: 493-496.
- Shah, P.S., J.P. Cannon, C.L. Sullivan, B. Nemchausky and C.T. Pachucki, 2005. Controlling antimicrobial use and decreasing microbiological laboratory tests for urinary tract infections in spinal-cord-injury patients with chronic indwelling catheters. Am. J. Health-Syst. Pharm., 62: 74-77.
- Abedin, M.Z., F. Yeasmin, S. Mia, H.B. Helal and R.Y. Shilpi, 2020. Bacteriological profile and antimicrobial susceptibility patterns of symptomatic urinary tract infection among patients of different age groups in a tertiary care hospital of Bangladesh. Moroccan J. Biol., 17: 59-66.
- Olowe, O.A., K.I.T. Eniola, R.A. Olowe and A.B. Olayemi, 2007. Starch paper technique is easy to detect beta lactamase detection from cases of diarrheagenic Escherichia coli in Osogbo. Life Sci. J., 4: 72-74.
- Drawz, S.M. and R.A. Bonomo, 2010. Three decades of β-lactamase inhibitors. Clin. Microbiol. Rev., 23: 160-201.
- Aziz, Q., Z. Ali, M. Izhar and V.H. Shah, 2012. Antimicrobial resistance; comparison of Escherichia coli in different areas of Lahore. Prof. Med. J., 19: 276-280.
- Nijssen, S., A. Florijn, M.J.M. Bonten, F.J. Schmitz, J. Verhoef and A.C. Fluit, 2004. Beta-lactam susceptibilities and prevalence of ESBL-producing isolates among more than 5000 European Enterobacteriaceae isolates. Int. J. Antimicrob. Agents, 24: 585-591.
- Mangaiarkkarasi, A., A.I. Erli and R. Gopal, 2013. Antimicrobial susceptibility patterns of clinical isolates of gram-negative pathogens from a teaching hospital, Pondicherry. Res. J. Pharm. Biol. Chem. Sci., 4: 664-673.
- Abdul Ghafur, A. Tayade and P. Kannaian, 2012. Clinical profile of patients treated with cefepime/tazobactam: A new β-lactam/β-lactamase inhibitor combination. J. Microbiol. Infect. Dis., 2: 79-86.
- Khan, F., A. Elhiday, I.F. Khudair, H. Yousef, O.A. Hussein, S.H. Alsamman and M. Elhamid, 2012. Evaluation of the use of piperacillin/tazobactam (Tazocin®) at Hamad General Hospital, Qatar: Are there unjustified prescriptions? Infect. Drug Resist., 5: 17-21
- Mavroidi, A., V. Miriagou, A. Liakopoulos, Ε. Tzelepi, A. Stefos, G.N. Dalekos and E. Petinaki, 2012. Ciprofloxacin-resistant Escherichia coli in Central Greece: Mechanisms of resistance and molecular identification. BMC Infect. Dis., 12.
How to Cite this paper?
APA-7 Style
Mia,
S., Masud,
M., Helal,
S.B., Rahman,
M.S., Refat,
M.R., Jarin,
L., Shilpi,
R.Y., Abedin,
M.Z. (2024). Isolation and Antibiotic Susceptibility of Escherichia coli from Urinary Tract Infections. Asian Science Bulletin, 2(2), 99-104. https://doi.org/10.3923/asb.2024.99.104
ACS Style
Mia,
S.; Masud,
M.; Helal,
S.B.; Rahman,
M.S.; Refat,
M.R.; Jarin,
L.; Shilpi,
R.Y.; Abedin,
M.Z. Isolation and Antibiotic Susceptibility of Escherichia coli from Urinary Tract Infections. Asian Sci. Bul 2024, 2, 99-104. https://doi.org/10.3923/asb.2024.99.104
AMA Style
Mia
S, Masud
M, Helal
SB, Rahman
MS, Refat
MR, Jarin
L, Shilpi
RY, Abedin
MZ. Isolation and Antibiotic Susceptibility of Escherichia coli from Urinary Tract Infections. Asian Science Bulletin. 2024; 2(2): 99-104. https://doi.org/10.3923/asb.2024.99.104
Chicago/Turabian Style
Mia, Samim, Mehedi Masud, Sumyea Binta Helal, Md. Sadiqur Rahman, Md. Abdur Rahman Refat, Laila Jarin, Rasheda Yasmin Shilpi, and Mohammad Zakerin Abedin.
2024. "Isolation and Antibiotic Susceptibility of Escherichia coli from Urinary Tract Infections" Asian Science Bulletin 2, no. 2: 99-104. https://doi.org/10.3923/asb.2024.99.104

This work is licensed under a Creative Commons Attribution 4.0 International License.